Презентацию на тему "Principles of paediatric anaesthesia"
можно скачать абсолютно бесплатно на нашем сайте. Предмет
проекта: Медицина. Красочные слайды и иллюстрации помогут вам
заинтересовать своих одноклассников или аудиторию.
Для просмотра содержимого воспользуйтесь плеером, или если вы хотите скачать доклад - нажмите на
соответствующий текст под плеером. Презентация
содержит 15 слайд(ов).
Слайд 1PRINCIPLESN OF PEDIATRIC ANAESTHESIA
Dr. Marovdi Vasyl-Banghazi Medical Center
Слайд 21.One of the most important differences between paediatric and adult patients is oxygen consumption which, in infants may exceed 6ml/kg/min, twice that of adults. 2.The cardiac index (defined as the cardiac output related to the body surface area to allow a comparison between different sizes of patients) is increased by 30-60 percent in neonates and infants to help meet the increased oxygen consumption 3.Stroke volume is therefore relatively fixed and the only way of increasing cardiac output is by increasing heart rate. 4.The sympathetic nervous system is not well developed predisposing the neonatal heart to bradycardia.

Слайд 3.Respiratory 1.The head is relatively large with a prominent occiput, the neck is short and the tongue is large. The airway is prone to obstruction because of these differences. 2.The epiglottis is large, floppy and U shaped. The trachea is short (approximately 4-9cm) 3.The glottic opening (laryngeal opening) is more anterior and the narrowest part of the airway is at the cricoid ring. (In the adult airway the narrowest point is the vocal cords). 4.An uncuffed endotracheal tube which has an air leak around it when positive pressure is applied to it should be used in children under 10 years of age. An uncuffed tube provides a larger internal diameter compared with a cuffed tube. 5.(Age / 2) + 12 6. Increased alveolar ventilation is achieved by an increase in respiratory rate

Слайд 4Temperature regulation 1.infants have a large surface area to volume ratio and therefore a greater area for heat loss, especially from the head. 2.There is an increased metabolic rate but insufficient body fat for insulation and heat is lost more rapidly. 3.It is important to maintain a warm environment to minimise heat loss.

Слайд 51.Fluid requirements can be considered as maintenance fluids and replacement fluids. 2.Maintenance fluid requirements are calculated on an hourly basis depending on the body weight. A suitable way of working this out is as follows: 4 ml/kg for the first 10 kg, adding 2 ml/kg for the second 10 kg and 1 ml/kg for each kg over 20 kg. A regimen with 30% of the fluid as normal saline and 70% as dextrose 5% is suitable for this purpose. 3.Replacement fluids.replaced by balanced salt solutions such as Hartmanns solution. Colloid solutions are sometimes used when losses are heavy.In general abdominal surgery will need extra fluid to replace these third space losses at around 10 mls/kg/hour for each hour of surgery

Слайд 6.Preoperative Assessment 1.Every patient should be visited by the anaesthetist prior to surgery, preferably in the presence of the parents in order to obtain a history, perform a physical examination and evaluate laboratory data in addition to estimating the patient's response to hospitalisation. 2.Fasting. Newborn to 12 months: No formula or breast milk 4 hours before surgery Clear liquids up to 2 hours before surgery Over 1 year: No formula, milk or solid food 6 hours before surgery Clear liquids up to 2 hours before surgery

Слайд 7Pre-medication 1.should be prescribed according to the needs of the patient. 2.Sedatives should be reserved for those who are unduly anxious. Oral midazolam 0.75 mg/kg administered 30 minutes prior to induction is very suitable. 3.Atropine or glycopyrrolate can be administered orally (or intramuscularly) preoperatively or given iv on induction of anaesthesia.Vagolytic dose of atropine (0.03 mg/kg) provides complete protection against vagal cardiac slowing or other cardiac arrhythmias.
Слайд 8Basic Anaesthetic Technique 1.Since children can deteriorate rapidly during anaesthesia it is especially important to check that all drugs and apparatus are ready prior to induction. 2.induction.Induction of anaesthesia is generally by intravenous or inhalational methods 3.Occasionally the anaesthetist is confronted by an unruly and hysterical child who will not co-operate with either of the above methods of induction. While an IM injection of ketamine (3-5 mg/kg) is possible

Слайд 9Pharmacology 1.Inhalational agents. Both induction and emergence from anaesthesia are more rapid in children than in adults. This is probably because of a smaller lung functional residual capacity per unit body weight and a greater tissue blood flow, especially to the vessel rich group (brain, heart, liver and kidney). Sevoflurane is a recently introduced inhalational agent which has the advantage of a pleasant non-irritating odour and a low blood/gas solubility coefficient. Consequently induction is both rapid and smooth and it is an ideal agent for inhalational induction but is considerably more expensive than halothane. 2.Intravenous Anaesthetics. An immature blood brain barrier and decreased ability to metabolise drugs may increase the neonate's sensitivity to barbiturates and opioids. Lower doses may be required to produce the desired pharmacological effects.

Слайд 10Anaesthesia breathing systems 1.Unintentional delivery of large tidal volumes to a small child can generate large airway pressures and cause barotrauma (damage to the lungs due to excessive inspiratory pressure). 2.Dedicated paediatric anaesthesia tubing is usually shorter and stiffer and the smaller tidal volumes can be better delivered manually with a 500 ml or 1000 ml breathing bag. 3.The efficiency of breathing circuits is measured by the fresh gas flow required to eliminate CO2 rebreathing. 4.The version most commonly used is the Jackson-Rees modification which has an open bag attached to the expiratory limb (classified as a Mapleson F system). Fresh gas flows of 2-3 times minute volume should be used to prevent rebreathing during spontaneous ventilation, with a minimum flow of 3 litres/min. During controlled ventilation the litres of fresh gas required per minute can be calculated by giving 1000 ml + 100 mls/kg. The minimum flow should be 3 litres/min.
Слайд 11Intra-operative Problem 1.Bradycardia in paediatrics often means hypoxia and restoring adequate ventilation and oxygenation may be all that is needed to restore heart rate 2.Bradycardia resulting from increased intracranial pressure is treated with hyperventilation, diuretics and surgical release of the pressure.

Слайд 12Basic Postoperative Care 1.Infants and children generally recover faster than adults from anaesthesia and surgery. 2.The child may return to the ward when the observations are stable, he is fully conscious and his pain is controlled. 3.Occasionally croup or subglottic oedema after endotracheal anaesthesia manifests itself in the first few hours after extubation.Mild cases will resolve over time and may only require extra observation and possibly some humidified oxygen.Nebulised adrenaline (5mg) by facemask is used in more severe cases.Steroids may or may not be useful and a single, large dose of i.v. dexa-methasone (4mg for infants, 8mg for children) can be used.If the above treatment is ineffective, preparations should be made for reintubation using a smaller endotracheal tube.

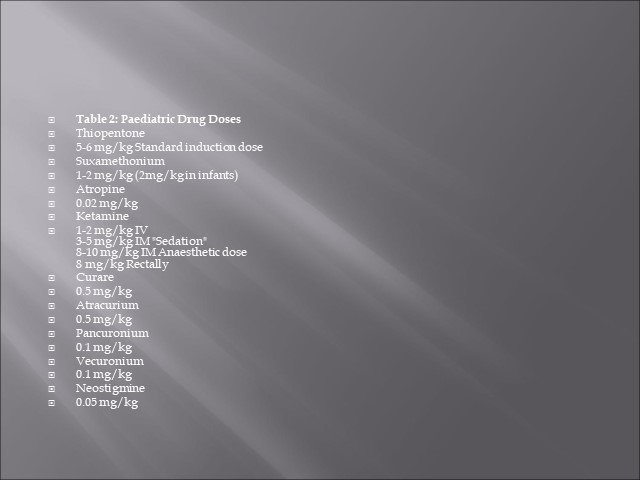
Слайд 13Table 2: Paediatric Drug Doses Thiopentone 5-6 mg/kg Standard induction dose Suxamethonium 1-2 mg/kg (2mg/kg in infants) Atropine 0.02 mg/kg Ketamine 1-2 mg/kg IV 3-5 mg/kg IM "Sedation" 8-10 mg/kg IM Anaesthetic dose 8 mg/kg Rectally Curare 0.5 mg/kg Atracurium 0.5 mg/kg Pancuronium 0.1 mg/kg Vecuronium 0.1 mg/kg Neostigmine 0.05 mg/kg
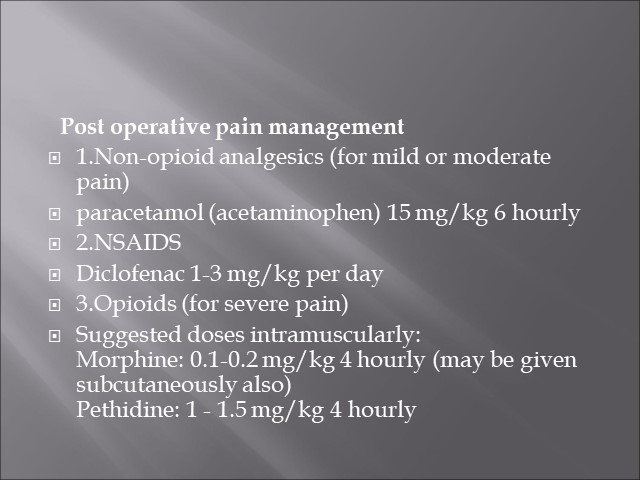
Слайд 14Post operative pain management 1.Non-opioid analgesics (for mild or moderate pain) paracetamol (acetaminophen) 15 mg/kg 6 hourly 2.NSAIDS Diclofenac 1-3 mg/kg per day 3.Opioids (for severe pain) Suggested doses intramuscularly: Morphine: 0.1-0.2 mg/kg 4 hourly (may be given subcutaneously also) Pethidine: 1 - 1.5 mg/kg 4 hourly
Слайд 15Thank you for attention